Hemighost cells
From haematologyetc.co.uk
AKA Blister cells
Derivation: From ancient Greek: prefix hemi (half); and descriptive term ghost cell: an empty cell whose outline remains visible
Appearance
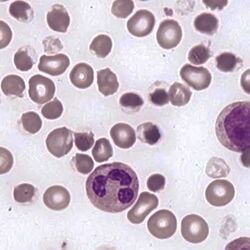
Cells where the haemoglobin is contracted to one pole of the cell leaving a visible empty area at the opposite pole surrounded by membrane (giving a characteristic “blister” appearance). In some cases, the haemoglobin may be entirely absent from the cell (ghost cell).
Images The typical appearance of a hemighost or blister cell, the haemoglobin is dense and is contracted to one pole of the cell to leave an area where membrane surrounds an “empty” area – the blister. This cell is a form of irregularly contracted cell which often accompany them
Significance
Hemighost cells arise when haemoglobin is damaged (similar to irregularly contracted cells with which they frequently co-exist). The hemighost appearance occurs particularly where there is oxidative damage and often indicates a deficiency of the protective enzyme glucose 6 phosphate dehydrogenase (which generates reducing power). The disorder particularly affects at-risk populations from Africa or Mediterranean origin). Hemighost formation therefore can be an acute event associated with progressive anaemia that requires immediate intervention. The presence of hemighost cells as a dominant feature should therefore be taken very seriously and reported urgently to clinical staff caring for the patient.
Pitfalls
The “blister” of empty membrane is the characteristic feature – once this is seen the recognition of hemighost cells is easy. Haemoglobin that forms crystals (e.g. HbC) can lead to cells that resemble hemighosts, but these lack of a clear blister (see section “Haemoglobin Crystals”). It is also important to realise that hemighost cells are rapidly removed by spleen and are often present only during the stage of active damage – afterwards there may only be anaemia and polychromasia.
Causes
| Related to enzyme deficiency |
|---|
| Deficiency of gluocose 6 phosphate dehydrogenase (G6PD) usually in the presence of an oxidative stress. |
| Realated to abnormal haemoglobin |
| Abnormal haemoglobin, particularly those that are unstable may cause the appearance, but generally the abnormal red cells will be infrequent in these causes. |
| Related to oxidative stress |
| A range of drugs and chemicals may cause oxidation – if the appearance is detected the clinician should take a careful clinical history |
Clinical Examples
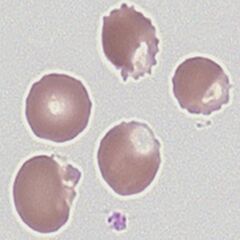
Clinical Image 1: The typical appearance of a hemighost (“blister cell”), the haemoglobin is dense and is contracted to one pole of the cell this leaves an area where membrane surrounds a part of the cell where haemoglobin is absent. Note in this case many cells present also have the appearance of irregularly contacted cells. Clinical condition: deficiency of G6PD with oxidative damage
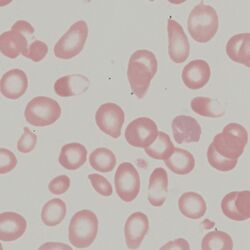
Clinical Image 2: In this instance the hemighost forms part of a wider range of irregularly shaped cells that include tear drop shapes (indicating a packed marrow) and also hypochromic and microcytic cells. This is an unusual unstable haemoglobin that also presents as a thalasaemia. Clinical condition: unstable haemoglobin
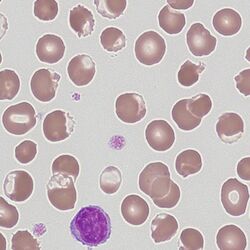
Clinical Image 3: This is s severe oxidative haemolysis in which hemighost cells can be easily seen, but note also an additional abnormal cell type is a red cells that contain no haemoglobin “ghost cells” reflecting the severity of the oxidative process. Clinical condition: severe oxidative haemolysis
Pathobiology
Damaged haemoglobin precipitates to form a focal mass at one pole of the cell, leaving an empty membrane-bound area. In severe forms haemoglobin is entirely removed from the cell forming an empty “ghost” cell. The hemighost appearance may coexist with other cells containing damaged haemoglobin – particularly irregularly contracted cells. In other cases, the denatured haemoglobin may form smaller “Heinz bodies” (these are not seen in normal stained films, but can be detected using appropriate extravital stains). Heinz bodies are removed by the spleen, following this removal residual spherocytes or keratocytes may be detected.